Pulmonary fibrosis: Symptoms, treatment, and outlook - Medical News Today
Pulmonary fibrosis (PF) is a type of interstitial lung disease that causes lung tissue to scar, thicken, and stiffen. It can make breathing difficult and interfere with oxygen absorption into the bloodstream.
Because of the way PF affects lung tissue, it causes a dry cough and shortness of breath. People living with PF can experience fatigue that results from decreased lung function.
This article reviews symptoms, causes, and risk factors for PF, as well as treatment options and lifestyle strategies a person can use to reduce symptoms.
Symptoms of PF resemble those of other lung diseases. They may include:
The American Lung Association states that there are more than 200 types of PF. In most cases, PF has no known cause — this is called idiopathic PF (IPF).
According to the Pulmonary Fibrosis Foundation, there are five main categories of PF that have causes a doctor can identify:
- Drug-induced: Certain medications, such as chemotherapy drugs, nitrofurantoin, amiodarone, and methotrexate, can affect the lungs and lead to PF.
- Radiation-induced: Chest radiation treatment can cause PF.
- Occupational: PF can result from exposure to certain vapors, fumes, fibers, and dusts, including those from asbestos, silica, and coal.
- Environmental: Also called hypersensitivity pneumonitis, this type of PF results from exposure to triggers, including mold and animals such as caged birds.
- Autoimmune: This type of PF relates to connective tissue disease and may accompany other symptoms such as skin changes, dry mouth or eyes, and joint inflammation.
Medical experts do not know the direct causes of IPF. However, several factors may increase a person's chances of developing this condition, including:
- Age: Most diagnoses occur in people in their
60s or 70s . - Sex: Males are more likely to develop IPF.
- Smoking: Tobacco use increases a person's chance of developing IPF.
- Genetics: A person has a higher risk of developing IPF if they have a first degree relative, such as a parent or sibling, who has the condition.
- Gastroesophageal reflux disease (GERD): Chronic GERD may contribute to IPF because of repeated aspiration of small amounts of reflux material into the lungs.
Certain gene mutations are common among people with IPF. Mutations can change the way a gene functions and may lead to unwanted effects.
Some of these mutations involve genes such as:
- MUC5B, which causes protective mucus to form in the lungs
- TERT and TERC, which produce the enzyme telomerase to protect DNA
Researchers estimate that variations in genetics account for about one-third of an individual's risk for developing IPF.
Treatment for PF can vary depending on the condition type and severity.
Medications
Doctors sometimes prescribe medications for PF, such as:
- nintedanib, an anti-fibrotic medication
- pirfenidone, an anti-inflammatory and anti-fibrotic drug for mild to moderate IPF
- tocilizumab, a biologic medication to prevent and treat inflammation
- immunosuppressant medications such as corticosteroids, mycophenolate mofetil, mycophenolic acid, and azathioprine
- medication for acid reflux to reduce the chance of stomach acid entering the lungs
- prescription or over-the-counter cough medicines
Oxygen therapy
Oxygen therapy, or supplemental oxygen, is a common treatment for PF.
Some people need this type of support all day, while others need oxygen only when they are physically active.
Doctors use a walking test to determine whether oxygen therapy might be helpful.
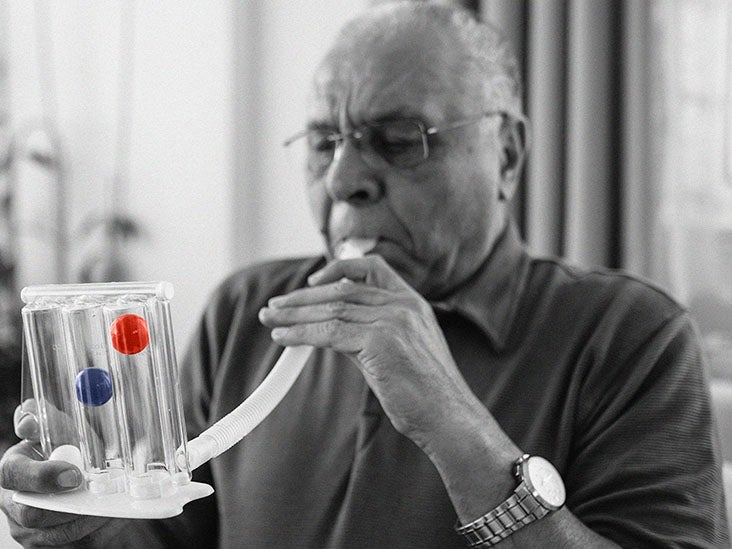
Pulmonary rehabilitation
Pulmonary rehabilitation is a combination of education and exercises designed to reduce symptoms and improve lung function.
Nurses and respiratory therapists work with people who have PF to develop skills such as energy conservation and to increase their activity level with less shortness of breath.
Lung transplant
A lung transplant is a treatment option for those who meet the eligibility requirements, which include:
- being in good physical condition
- having no other life threatening illness
- being willing to accept the surgical risks
- accepting post-transplant therapy
Clinical trials
Clinical trials assess the safety and effectiveness of experimental treatments.
Participants gain access to new treatment options and the opportunity to help support PF research.
Lifestyle strategies
A person with PF may benefit from the following lifestyle strategies:
- protecting the lungs from irritants such as dust and chemicals
- seeking support to quit smoking, if necessary, and avoiding exposure to secondhand smoke
- engaging in regular, moderate exercise, such as walking
- reaching and maintaining a healthy BMI
- eating a heart-healthy diet and aiming for smaller and more frequent meals
- staying up to date on vaccines, including those for the flu, pneumonia, and COVID-19
It is also important to take care of one's mental health. In addition to reaching out to family and friends for support, a person can try counseling or a support group for people with PF.
A person can find a support group here.
Because its symptoms are similar to those of other lung conditions, PF can be challenging to diagnose. Consulting a specialist can help ensure that a person gets the correct diagnosis.
PF diagnosis involves several steps:
- Health history and physical exam: A health history reveals important information, including whether a person has family members with lung disease and whether a person has had exposure to airborne materials that can contribute to PF. During a physical exam, a doctor can look for signs of PF.
- Lung function tests: These tests measure factors such as the capacity of the lungs, how well they move air, and how well they transfer blood gases such as oxygen and carbon dioxide.
- Imaging tests: These tests can reveal the presence of scarring in lung tissue.
- Tissue samples: Tests that doctors can use to obtain tissue samples include a bronchoscopy, bronchoalveolar lavage, thoracoscopic surgery, and thoracotomy.
- Blood tests: These tests can check for co-occurring conditions such as joint disorders and autoimmune conditions. They can also check the function of the liver and kidneys.
- Tuberculosis (TB) test: TB and PF have similar symptoms, so the doctor may want to conduct a skin or blood test for TB.
- Genetic testing: This type of test can determine whether a person has gene mutations with links to PF.
PF can sometimes lead to complications such as:
Sometimes complications can lead to an acute exacerbation, which is a rapid decrease in lung function. An acute exacerbation can also occur without an identifiable cause.
PF is chronic and progressive, and it can reduce the expected length of a person's life. The average amount of time a person may live after a PF diagnosis is 3–5 years. However, this is just an average, and life expectancy can vary.
Having a lung transplant can change the life expectancy of a person living with PF. The amount of change depends on the success of the transplant.
There is no way to prevent PF, but avoiding potential causes is one way to reduce the risk of developing this condition.
Treating underlying conditions that can affect the lungs, such as GERD, can also help.
PF is a chronic, progressive disease that can reduce a person's life span. Although PF is not preventable, knowing some of the causes can help a person reduce their chance of developing it.
People who live with PF can manage their symptoms with medication, lifestyle strategies, oxygen therapy, and pulmonary rehabilitation.
For those who meet the eligibility requirements, a lung transplant may be another treatment option.


Comments
Post a Comment