Aortic Stenosis: Diagnosis, Symptom Progression, Surgery
Coronary Artery Disease
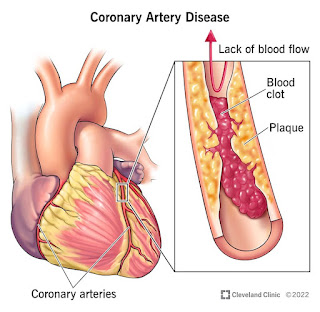
Coronary artery disease (CAD; also atherosclerotic heart disease) is the end result of the accumulation of atheromatous plaques within the walls of the coronary arteries that supply the myocardium (the muscle of the heart) with oxygen and nutrients. It is sometimes also called coronary heart disease (CHD). Although CAD is the most common cause of CHD, it is not the only one.
CAD is the leading cause of death worldwide. While the symptoms and signs of coronary artery disease are noted in the advanced state of disease, most individuals with coronary artery disease show no evidence of disease for decades as the disease progresses before the first onset of symptoms, often a "sudden" heart attack, finally arises. After decades of progression, some of these atheromatous plaques may rupture and (along with the activation of the blood clotting system) start limiting blood flow to the heart muscle. The disease is the most common cause of sudden death, and is also the most common reason for death of men and women over 20 years of age. According to present trends in the United States, half of healthy 40-year-old males will develop CAD in the future, and one in three healthy 40-year-old women. According to the Guinness Book of Records, Northern Ireland is the country with the most occurrences of CAD. By contrast, the Maasai of Africa have almost no heart disease.
As the degree of coronary artery disease progresses, there may be near-complete obstruction of the lumen of the coronary artery, severely restricting the flow of oxygen-carrying blood to the myocardium. Individuals with this degree of coronary artery disease typically have suffered from one or more myocardial infarctions (heart attacks), and may have signs and symptoms of chronic coronary ischemia, including symptoms of angina at rest and flash pulmonary edema.
A distinction should be made between myocardial ischemia and myocardial infarction. Ischemia means that the amount of blood supplied to the tissue is inadequate to supply the needs of the tissue. When the myocardium becomes ischemic, it does not function optimally. When large areas of the myocardium becomes ischemic, there can be impairment in the relaxation and contraction of the myocardium. If the blood flow to the tissue is improved, myocardial ischemia can be reversed. Infarction means that the tissue has undergone irreversible death due to lack of sufficient oxygen-rich blood.
An individual may develop a rupture of an atheromatous plaque at any stage of the spectrum of coronary artery disease. The acute rupture of a plaque may lead to an acute myocardial infarction (heart attack).
Coronary Artery Disease And Coronary Bypass Surgery
Content
During this operation, the surgeon will make an incision, called a median sternotomy, in your chest and through the breastbone.
They will take healthy vessels from another part of your body to 'bypass' the blocked arteries that are preventing oxygenated blood from efficiently reaching your heart. A healthy artery in your chest may be used, or veins from your leg can be taken and used to bypass the blockage. In order for your surgeon to obtain the healthy veins, one or two small incisions are made in the leg.
During most open-heart surgeries it is necessary to connect you to a heart-lung bypass machine. During this time, your heart will stop. This machine takes over the work of the heart, oxygenating your blood and circulating it throughout the body. Your heart will begin beating again once the procedure is complete.
Dear Doctor: Why Aren't Angioplasties, Stents Used More Often In Patients With Coronary Artery Disease?
DEAR DR. ROACH: I am 68 and in good shape; I work out daily. I had a few episodes of angina two to three years ago and started going to a cardiologist as a result. I have had quite a few tests done, but the one that was really concerning was my coronary artery calcium score, which is over 4,800 (not a misprint).
He put me on 80 mg of atorvastatin, 10 mg of ezetimibe and 40 mg of valsartan. My blood pressure is good (generally around 110 over 65 mm Hg), and other than some shortness of breath, I feel fine. I'm wondering if my doctor should be more aggressive due to the extremely high CAC score (i.E., a stent). I would really like to hear your thoughts about this. -- C.B.
ANSWER: Your extremely high calcium score means you are at a very high risk for, and probably have, blockages in the arteries that provide blood to the heart muscle. This condition is called coronary artery disease (CAD).
There are several medications that have been proven to reduce the risk of heart attack and death in people with coronary artery disease: statins (80 mg of atorvastatin is the highest dose of one of the most effective statins); ezetimibe (which works along with the statin to stabilize blockages); and ACE inhibitors and angiotensin blockers (valsartan probably has benefits beyond lowering blood pressure to prevent heart disease), all of which you are on. If your doctor was sure that you really have CAD, you should probably be on aspirin and a beta blocker as well, unless there is an underlying reason not to be.
Although stents are commonly placed after cholesterol plaque blockages are opened through a balloon procedure, they have not been proven, despite many studies, to reduce the risk of heart attack and death in people who have stable coronary artery disease. (The story is different for people who experience an emergency like a heart attack.)
Angioplasties and stents are normally reserved for people who have symptoms of heart blockages that have not been treated successfully with medications. A recent and still controversial study cast doubt on how effective stents are at relieving symptoms.
I can't tell if your shortness of breath is a symptom due to blockages of the heart. A cardiologist's clinical judgment is necessary to determine whether a test, such as an angiogram, is appropriate to see how many blockages there are and their severity. Although a CT scan with dye can give excellent information, an angioplasty and stent placement can only be done during a cardiac angiogram.
In a few cases, the blockages are so severe that a decision is made to go directly into surgery, where one or more grafts can be placed to bypass the blockages found on the angiogram. There are specific indications for cardiac surgery. Medications are much more effective than they used to be, so there are far fewer coronary artery bypass graft surgeries (CABG, always pronounced "cabbage") performed now than in decades prior.
* * *
Dr. Roach regrets that he is unable to answer individual letters, but will incorporate them in the column whenever possible. Readers may email questions to ToYourGoodHealth@med.Cornell.Edu or send mail to 628 Virginia Dr., Orlando, FL 32803.
(c) 2022 North America Syndicate Inc.
All Rights Reserved
If you purchase a product or register for an account through a link on our site, we may receive compensation. By using this site, you consent to our User Agreement and agree that your clicks, interactions, and personal information may be collected, recorded, and/or stored by us and social media and other third-party partners in accordance with our Privacy Policy.



Comments
Post a Comment